Drug allergies present a complex landscape, demanding tailored management strategies based on the reaction’s nature and severity. We’ve witnessed significant progress in “de-labeling” allergies to common drugs like penicillin through careful testing, allowing many to safely access essential treatments. However, the approach to severe cutaneous adverse reactions (SCARs) – encompassing Stevens-Johnson Syndrome (SJS), Toxic Epidermal Necrolysis (TEN), Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS), and Acute Generalized Exanthematous Pustulosis (AGEP) – often stands in stark contrast: a broad and often indefinite avoidance of all potentially implicated drugs.
While the inherent caution surrounding SCARs is understandable given their potential severity, this blanket approach may inadvertently limit crucial treatment options. Could a more nuanced, risk-based strategy offer a better balance, prioritizing patient safety while preserving access to necessary medications?
Learning from the Other End: The Success of Direct Provocation
The management of penicillin allergy offers a valuable parallel. For patients with low-risk histories, direct drug provocation – the supervised reintroduction of the drug – has become a cornerstone of care. Guided by evidence-based risk stratification algorithms like PEN-FAST, this approach helps confirm or exclude true allergies, reducing unnecessary avoidance and ensuring appropriate antibiotic use. This success in targeted drug reintroduction highlights the potential benefits of a more selective approach in drug allergy management.
The “Wall of Fear” Around SCARs: Is It Always Justified?
In the aftermath of a SCAR, the immediate priority is to discontinue all suspect medications. However, this often translates into long-term avoidance of multiple drugs administered around the time of the reaction, despite evidence suggesting that only one or two are typically the actual culprits, with others being coincidental exposures.
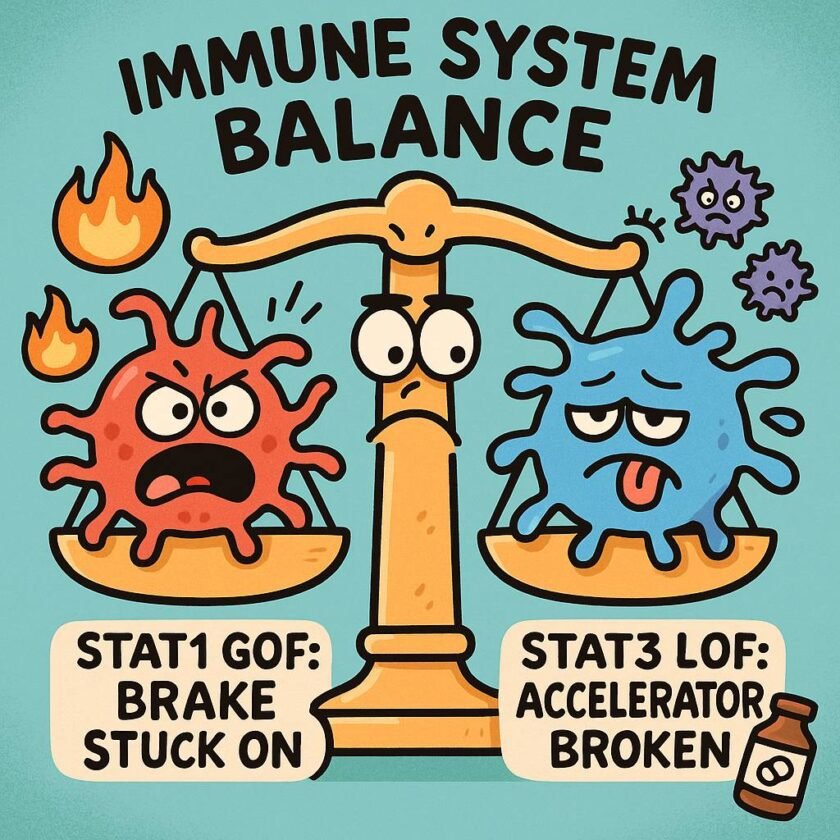
While the fear of rechallenging a severe reaction is significant, this overly cautious stance can have profound consequences, denying patients access to essential medications they may not be allergic to. Furthermore, SCARs exhibit considerable heterogeneity:
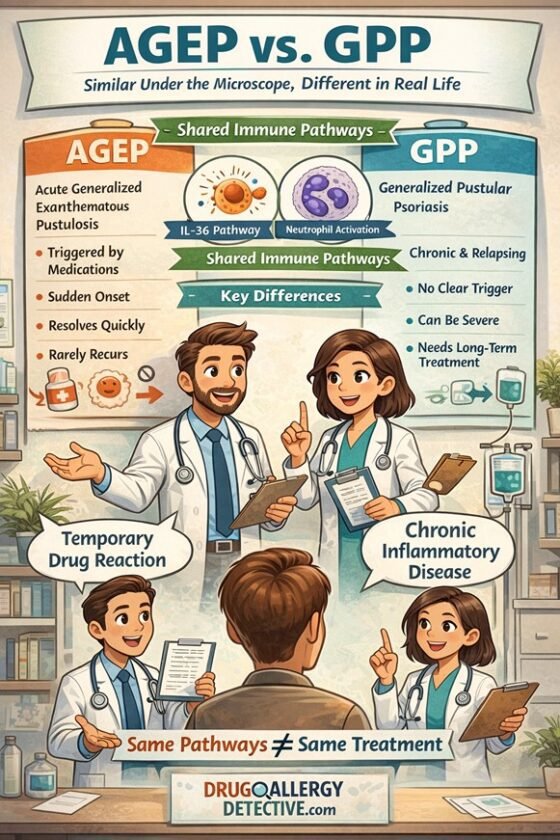
- Acute Generalized Exanthematous Pustulosis (AGEP) often presents as a milder, self-limiting condition.
- Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS) displays a spectrum of severity, ranging from mild skin involvement to severe multi-organ dysfunction.
- Toxic Epidermal Necrolysis (TEN) is a life-threatening dermatologic emergency requiring strict avoidance of the causative agent.
Treating all SCARs uniformly fails to acknowledge this variability. Moreover, conditions mimicking SCARs, such as reactive infectious mucocutaneous eruption (RIME), can lead to misdiagnosis and unnecessary drug restrictions.
A Critical Gap: The Need for Risk Stratification Algorithms in SCARs
The success of risk stratification in managing penicillin allergy prompts the question: could a similar approach be applied to SCARs?
For Stevens-Johnson Syndrome (SJS) and Toxic Epidermal Necrolysis (TEN), the ALDEN algorithm provides a valuable tool. It estimates the probability of a specific drug being the culprit based on the latency period, the timing of drug initiation, and the drug’s known association with these conditions.
However, a critical limitation exists: the ALDEN algorithm is specifically designed and validated for SJS and TEN and is not applicable to DRESS or AGEP. Currently, there are no equivalent, validated algorithms to aid in determining drug causality for these other significant SCAR phenotypes. This lack of standardized tools presents a major obstacle to implementing a more nuanced and personalized management strategy for all SCARs. Developing and validating such algorithms is a crucial step forward.
Toward Risk Stratification in SCARs: A Potential Framework
Despite the current limitations, the principles of risk stratification could still guide a more refined approach to SCARs management, considering:
- The likelihood of a specific drug being the true cause: While the ALDEN algorithm currently only applies to SJS/TEN, careful clinical assessment of the timeline, reaction features, and drug characteristics remains essential for all SCARs.
- The severity of the SCAR phenotype: Assessing the extent of skin involvement, systemic manifestations, potential long-term sequelae, and underlying comorbidities is crucial.
- The availability and necessity of alternative medications.
- The potential role of diagnostic tools: In select cases, in vitro tests like IFN-gamma ELISpot and Lymphocyte Transformation Tests (LTT), and cautiously performed skin tests, might offer additional insights.
Based on these factors, a more tailored approach could emerge:
- Low-likelihood culprit drug + milder SCAR (e.g., AGEP): In specific, carefully evaluated circumstances, a supervised graded challenge might be considered.
- Intermediate cases: Further investigation using available diagnostic tools and careful clinical judgment is warranted.
- High-likelihood culprit drug (e.g., ALDEN ≥ 4 in SJS/TEN) + severe SCAR (e.g., TEN, severe DRESS): Permanent avoidance remains the safest and most prudent course of action.
Emerging Evidence: Rechallenge is Not Always Dangerous
Challenging the traditional stance of absolute avoidance, emerging data from regions like South Africa and South Korea suggest that drug rechallenge in carefully selected SCAR patients can be feasible, particularly when alternative treatments are limited. These findings highlight the potential for a more individualized approach.
Conclusion: Moving Toward Personalized and Evidence-Based SCAR Management
The current management of drug allergies often presents a stark contrast between the proactive testing in milder reactions and the broad avoidance in SCARs. While the need for caution in SCARs is undeniable, our practices may benefit from a more nuanced, evidence-based approach.
A shift toward risk stratification, incorporating a thorough assessment of causality (utilizing tools like ALDEN where applicable and striving for similar tools for other SCARs), the severity of the reaction, and the individual patient’s needs, offers a more balanced path forward. By embracing this perspective, drug allergy management—even in the context of severe reactions—can become not only safer but also more rational, personalized, and ultimately optimized for patient care.
References
Chongpison, Y., Sriswasdi, S., Buranapraditkun, S., Thantiworasit, P., Rerknimitr, P., Mongkolpathumrat, P., … & Klaewsongkram, J. (2024). IFN-γ ELISpot-enabled machine learning for culprit drug identification in nonimmediate drug hypersensitivity. Journal of Allergy and Clinical Immunology, 153(1), 193-202.
Disclaimer
Drug rechallenges in SCARs should only be performed by specialists. They should be considered only when the suspected drugs are essential for treatment and must always involve informed consent from the patient.

[…] […]